Rutgers study sheds light on why some tuberculosis strains are more severe, transmissible
A recent Rutgers study found that two strains of tuberculosis bacteria, despite having only slightly different genetics, resulted in greatly different disease development and transmissibility, according to a press release.
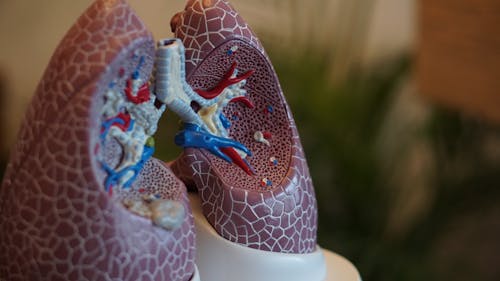
The study focused on how two strains of mycobacterium tuberculosis — one strain categorized as high transmission (Mtb-HT) and the other as low transmission (Mtb-LT) — can affect lungs differently.
When performing the study, Rutgers researchers used mice to understand the differences in immune response that different strains cause in their lungs, according to the release.
The results showed that mice infected with the Mtb-HT strain formed clumps of alveolar macrophages (AMs) or immune cells in their lungs.
These clumps are referred to as granulomas, which envelope the invading bacteria to prevent more serious diseases, according to the release.
Though, typically the granulomas would break down at one point and release the bacteria back into the lungs.
Researchers suspect that if these infectious bacteria found themselves close to the lung’s bronchi, they could escape out into the air and cause more infection — increasing the strain's transmissibility, according to the release.
Conversely, mice infected with the Mtb-LT strain produced inflammation within the lungs that did not allow bacteria to leave the lungs into the air, thereby causing a more intense tuberculosis infection.
Essentially, the study demonstrated that the Mtb-HT strain caused less virulent disease with greater transmissibility while the Mtb-LT strain led to a more virulent disease with lower transmission, according to the study.
The reason behind the divergences in disease intensity and transmissibility is how the bacteria interact with the lung’s AMs.
Mice infected with the Mtb-HT strain had faster AM movement into the interstitium, triggered by Interleukin-1 receptor (IL-1R) signaling.
This allowed for more effective T helper type 1 (Th1) cell priming and granuloma formation within the lung, which fought off the disease, according to the study.
On the other hand, mice with the Mtb-LT strain experienced delayed AM migration to the interstitium, causing reduced Th1 priming and a lack of granulomas.
The study found that this was due to the Mtb-LT strain manipulating IL-1R signaling to make disease symptoms more severe, according to the study.
Padmini Salgame, associate director of the Public Health Research Institute at Rutgers New Jersey Medical School (NJMS) and study co-author, said collecting the two strains themselves was a challenge.
“Conducting the household contact study and obtaining the Mycobacterium tuberculosis strains required tremendous team effort from a large group of investigators from two different countries and with varying scientific expertise,” she said.
Salgame said the findings demonstrate that tuberculosis treatments may be more successful if they took into account each patient’s strain of infection.
Additionally, she said the study raises the possibility as to whether in addition to drugs, tuberculosis treatment can include therapies that target specific immune pathways.
Salgame also said the researchers were surprised by the important role that AMs and IL-1R signaling played in Th1 priming and granuloma formation.
Jerrold Ellner, director of Research Innovations for the Center for Emerging and Re-Emerging Pathogens at NJMS and study co-author, shared similar sentiments.
“The dogma is that characteristics of the human host and the environment determine whether (tuberculosis) infection is transmitted to close contacts,” he said. “We found rather that certain bacterial strains were transmitted well and others poorly.”



